Capitol Beat
Winging it: How government agencies are fighting bird flu
COVID, quarantines, worst- and best-case scenarios: behind the scenes of Pennsylvania’s fight against avian flu and the next pandemic.

catnap72 via Getty Images
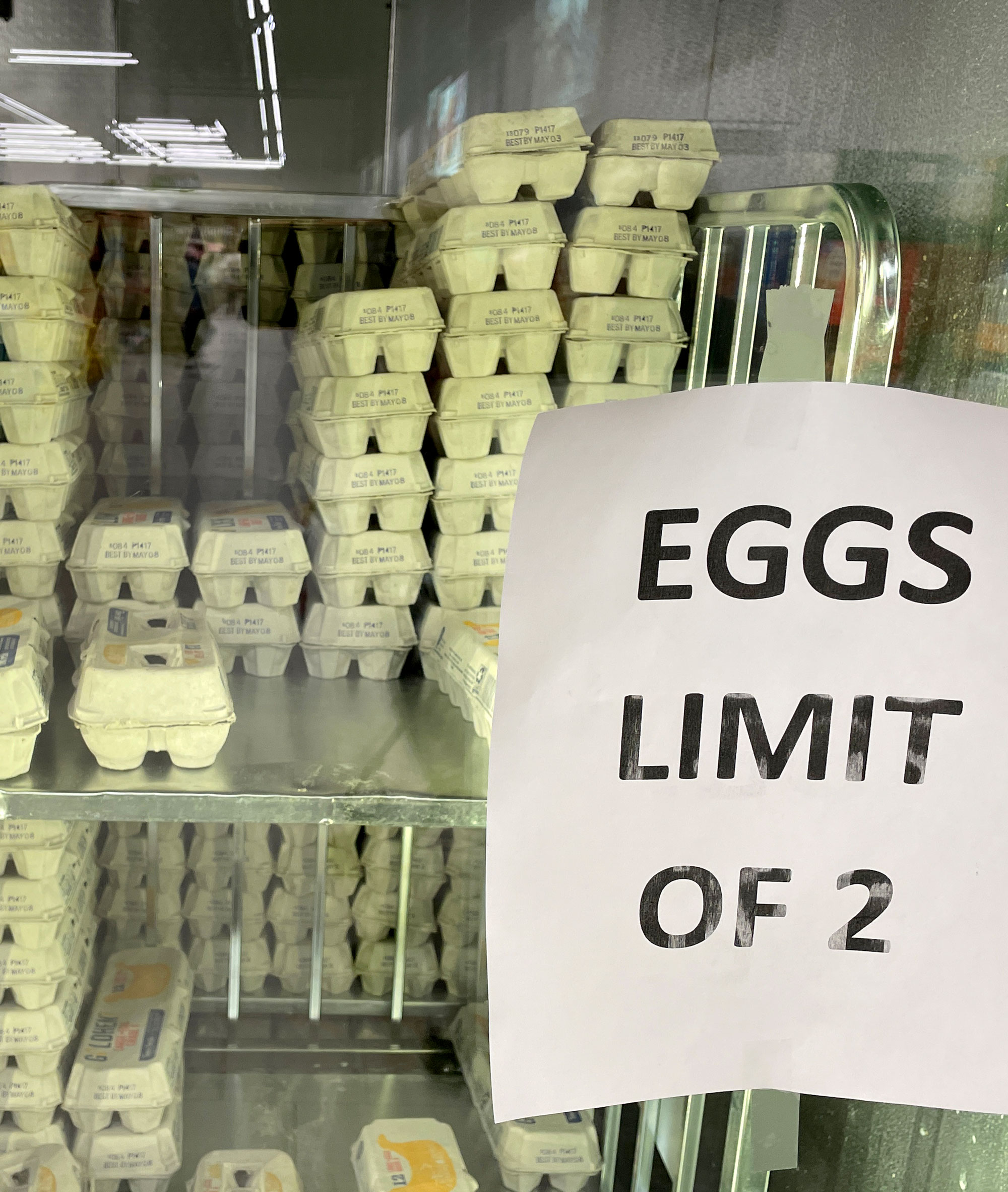
It’s been just five years since COVID-19 came on the scene, killing more than 7 million people worldwide, upending life across the globe. But today, it’s an older, more familiar virus that is attracting the attention of state officials and public health leaders.
Since it emerged in Pennsylvania in 2022, highly pathogenic avian influenza – also known as HPAI, H5N1 or bird flu – has been detected in wild and commercial flocks throughout the state, bringing about concerns that H5N1 could damage the state’s agricultural economy.
It’s also mobilized public health leaders, who say that while avian influenza’s risk to humans is low right now, the virus is worth monitoring for its pandemic potential.
“The message has been consistent: The risk to the average person is low,” Dr. Jaan Naktin, an infectious disease expert at Lehigh Valley Health Network, told City & State in an interview. “I would echo that concern to any of my patients, or any other forum I would talk in: The risk is low.”
Bird flu, explained
Highly pathogenic avian influenza is a virus that is highly contagious and deadly among birds. To date, it has also been detected in several other species, including dairy cattle, wild and domestic cats, red foxes and even bottlenose dolphins, according to the Centers for Disease Control and Prevention.
There are two main types of avian influenza: highly pathogenic avian influenza and low-pathogenicity avian influenza. Low-pathogenicity avian influenza, referred to as LPAI, occurs naturally in waterfowl and shorebirds without causing illness. Highly pathogenic avian influenza, better known as HPAI, is much more infectious, can spread rapidly between flocks and is often fatal to domestic birds, according to the U.S. Department of Agriculture’s Animal and Plant Health Inspection Service.

Birds that have been infected with HPAI can experience a lack of energy and appetite, decreased egg production, soft-shelled or misshapen eggs, swelling of the head, comb, eyelids, wattles and hocks, as well as nasal discharge and coughing and sneezing. HPAI can also result in sudden death for infected birds.
Since 2024, the virus has been detected in 70 humans, with the bulk of the cases occurring in California, Colorado and Washington among those who work closely with commercial dairy and poultry operations. Louisiana reported the first and only H5N1 death among humans in the United States in early January. However, in Pennsylvania, there have been no infections among humans or dairy cattle as of early April, according to the Pennsylvania Department of Agriculture.
In humans, avian influenza symptoms can seem similar to the regular flu, with sore throat, headache, fatigue, fever and muscle aches all being common symptoms of H5N1. What sets H5N1 apart from more common strains of influenza is that it can cause conjunctivitis or redness of the eyes in humans who have been infected, according to the CDC.
State government response efforts
Officials have been actively monitoring the spread of bird flu in Pennsylvania since the initial case was detected at a commercial poultry farm in Lancaster County in April 2022. Following the first positive tests, the Pennsylvania Department of Agriculture established quarantine zones around impacted farms, implemented strict biosecurity measures and euthanized infected birds.
That work has continued. Following the detection of avian influenza at a Lehigh County commercial poultry farm in January, the department said each farm with a presumed positive will be quarantined, and that all commercial poultry facilities within a 10-kilometer radius will be subject to testing requirements and limitations on the transportation of poultry products.
The state also has a dedicated fund to help farmers and others in the agricultural industry recover from bird flu-related damages. The HPAI Recovery Reimbursement Grant program offers awards of up to $25,000 to help applicants improve biosecurity measures aimed at reducing the spread of H5N1 on farms.
Gov. Josh Shapiro recently highlighted the program and his administration’s work on HPAI during an appearance at the Pennsylvania Farm Bureau’s annual state legislative luncheon.
“We are the only state in the nation with this type of dedicated funding to help our poultry farmers get back up on their feet,” Shapiro told the gathering, while also touting his administration’s work to open up a new state testing laboratory in Beaver County, which he said would “expand our testing capacity and help mitigate future disease outbreaks.“
The governor also celebrated his administration’s efforts to aggressively test dairy milk. The Pennsylvania Department of Agriculture announced in February that it reached “HPAI-free” status under the U.S. Department of Agriculture’s National Milk Testing Strategy, which Agriculture Secretary Russell Redding said in February was a testament to collaborative work between the Shapiro administration and the legislature. “Gov. Shapiro and the General Assembly’s support through quick, responsive funding for virus elimination and testing,” he said, “and grants to cushion losses to the industry have kept Pennsylvania poultry thriving amid immense, unprecedented challenges.”

Shapiro added that the state has millions left in the recovery fund as the threat from H5N1 persists.
“We've only had to spend $13 million to help our poultry producers cover the cost they incurred in responding to outbreaks on their farms, which leaves us today … with $61 million in our (highly pathogenic) avian influenza fund to be able to support our farmers,” he told the Farm Bureau, noting that the sum is “more than enough to meet the needs of our poultry farmers and see them through this crisis.”
“Should we need more? You have my word: I will be there to make sure our poultry farmers have what they need to get back up on their feet again,” the governor added.
H5N1’s impact on public health
Infectious disease experts say that while the virus could mutate and become more of a threat to humans, it isn’t at that point yet.
According to the CDC, there has been no human-to-human transmission in the U.S. to date, and experts who spoke with City & State acknowledged that there is an existing vaccine stockpile for avian influenza – something that wasn’t true at the onset of the COVID-19 pandemic.
“There is a national stockpile right now of several million doses of vaccine that appears to be active to the current strains that are out there,” said Dr. Jeffrey Jahre, an infectious disease specialist at St. Luke’s University Health, a nonprofit health network that serves the Lehigh Valley region. “That’s important because, obviously, you want to get a head start. If we find that all of a sudden a change in (how) humans are infected, are a couple of million strains going to be adequate? No, they’re not. But we do have methods of ramping up production that would be primarily the mRNA vaccines.”
Both Jahre and Naktin said that another key difference between the COVID-19 pandemic and the threat posed by avian influenza is that H5N1 appears to be susceptible to readily available flu medications like Tamiflu. “There is a national stockpile of several 100 million doses of that. So we’re not totally unprepared,” Jahre added.
Researchers from the University of Pittsburgh and the National Institutes of Health Research Center wrote in a Jan. 30 article that a prophylactic antibody-based immune therapy has protected monkeys against H5N1 – a finding that the university said in a January press release “sets the stage for the development of medical countermeasures against future influenza virus pandemics.”
One note of caution comes from a study done by researchers in Texas, who appear to have found a human-isolated strain of H5N1 with mutations that “enable it to replicate more efficiently in human cells and cause severe disease in mice,” according to a 2025 article published in the American Journal of Managed Care.
Still, as things stand right now, it would likely take more mutations for the virus to have a greater impact on humans. “We don’t even know if it jumps from animals to humans, if it’s really gonna go human-to-human,” Naktin said. “So that’s a whole other step, mutation-wise, that has to occur before we have that situation.”
Jahre concurred, noting that while now is not the time to sound the alarm on avian influenza, it’s important to continue tracking and monitoring the virus as it spreads across the commonwealth – and the globe.
“What's important in terms of humans is that there has been no human-to-human transmission yet. There has been, obviously, different interspecies transmission in animals,” he said. “Whenever you see that ability, there is always a worry because we know that there have been mutations in this virus, that it can change from something that is relatively non-threatening to humans right now – that can change with a set of mutations. We know that this virus has the ability to do that.”
“So whereas there's certainly no reason to panic, there is also no reason to be absolutely complacent,” he said.
